A Quiet Night That Changed Everything
It began like any other night. The air was calm, the lights dim, and two people — partners who had shared countless evenings together — climbed into bed without a second thought. It was the kind of ordinary moment that defines life: routine, comfortable, safe.
But sometimes, danger doesn’t come with a warning. Sometimes, it hides quietly in the places we feel most secure.
By morning, what began as an unremarkable night would end in devastation. What unfolded in the stillness of those hours would leave one family shattered, their friends in disbelief, and millions of readers online struggling to comprehend how something so innocent could end so tragically.
The story spread like wildfire across social media. At first, the details were vague — just a headline about a couple and a tragic accident during sleep. Then came speculation, comments, and expert opinions. Within days, it became more than a single story. It became a wake-up call about the silent dangers that can turn rest into risk — and the fragile nature of the human body when it is most vulnerable.
The Unimaginable Discovery

When emergency responders arrived, the scene was eerily peaceful. One person lay still, the other distraught, unable to process what had just happened. The air was heavy with disbelief. According to first responders, there were no signs of struggle, no indication of foul play — only the quiet aftermath of a medical event that struck without warning.
For those involved, it was almost impossible to accept. “They had gone to bed like any normal couple,” one family member told local reporters. “They were healthy, happy, and there was no reason to think something like this could happen.”
Investigators later determined that the tragedy likely stemmed from a medical emergency that occurred while one person was asleep, such as cardiac arrest, respiratory failure, or complications from undiagnosed sleep disorders. The realization was heartbreaking: the body, even in its most restful state, is not immune to sudden danger.
This wasn’t a story about negligence or recklessness. It was a story about fragility — about how the line between safety and tragedy can blur in the quietest of moments.
The Ripple of Shock and Sorrow
News of the incident spread rapidly. Within hours, social media feeds filled with condolences, questions, and disbelief. Friends and acquaintances shared photos of the couple — smiling, laughing, living life — and struggled to understand how something so ordinary could end so abruptly.
“They were inseparable,” one friend wrote. “You couldn’t meet a kinder pair.”
But amid the grief, people began to share their own experiences — stories of sleep apnea, heart complications, or other nighttime emergencies that had gone unnoticed until it was almost too late. What began as a tragedy soon became a mirror for thousands of others to reflect on their own habits, their loved ones, and their vulnerability in sleep.
Doctors and sleep specialists started weighing in, explaining that while we think of sleep as peaceful, it is also one of the body’s most complex and delicate states. During those hours, heart rate, breathing, and muscle activity all change dramatically — and even minor imbalances can have serious consequences.
The Science of Silent Danger
To understand how such tragedies occur, it helps to look closer at the science of sleep. When we fall asleep, our bodies shift into a restorative mode — muscles relax, breathing slows, and the brain cycles through distinct phases of rest.
For most people, this process is uneventful and essential. But for some, underlying health conditions can transform sleep into a hidden risk.
Sleep Apnea — The Breathing Threat
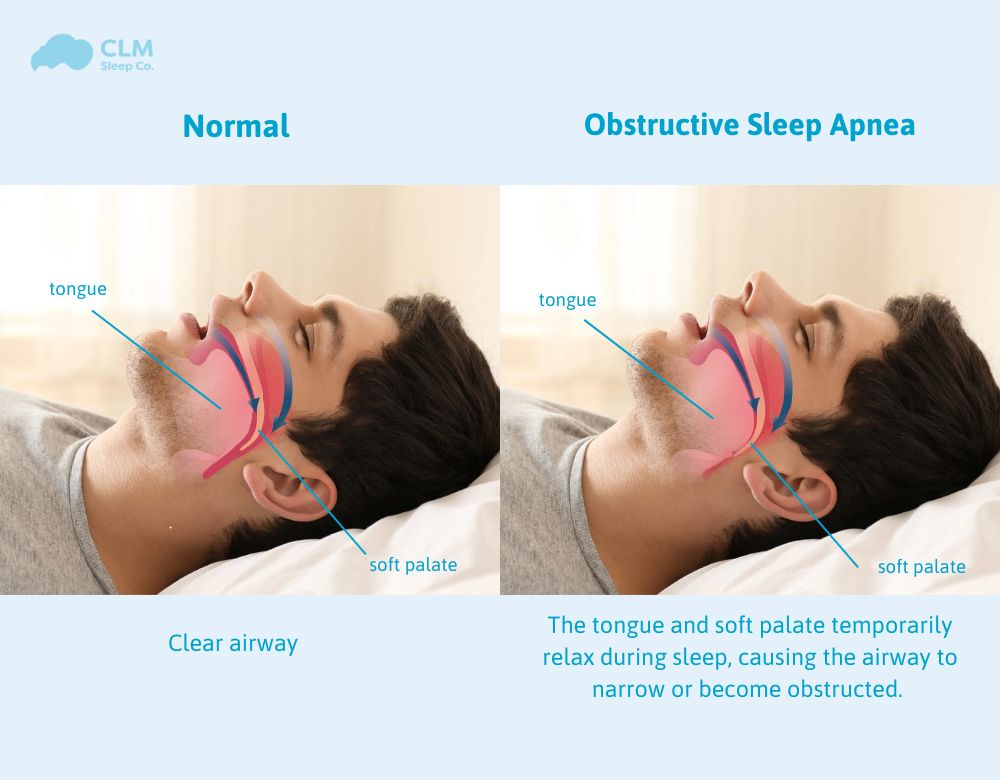
One of the most common and potentially dangerous sleep disorders is obstructive sleep apnea (OSA), which affects millions of people worldwide. In OSA, the muscles of the throat relax too much during sleep, causing the airway to collapse. Breathing temporarily stops — sometimes dozens or even hundreds of times per night.
Dr. Emily Rhodes, a sleep medicine specialist at the Mayo Clinic, explains:
Final Diagnosis: Sweet Syndrome
Histopathological analysis of the skin biopsy confirmed Sweet Syndrome. The diagnosis was based on both clinical presentation and tissue findings, characterized by dense neutrophilic infiltrates in the dermis without vasculitis.
This case highlights the rare occurrence of Sweet Syndrome following inhaled bronchodilator therapy—specifically, a combination of indacaterol and glycopyrronium, which has not previously been reported in medical literature as a trigger for this condition.

What Is Sweet Syndrome?
Sweet Syndrome is classified among neutrophilic dermatoses. It typically presents with:
- Painful erythematous plaques or nodules
- Sudden onset
- Fever
- Leukocytosis
The lesions are often bilaterally distributed and asymmetrical, typically affecting the face, neck, upper trunk, and extremities.
Common Symptoms:
- Low-grade to moderate fever
- Painful skin lesions (papules or plaques)
- Fatigue or malaise
- Joint pain or ocular symptoms (in some cases)
Diagnostic Criteria for Sweet Syndrome
According to Su and Liu (1986) and updated clinical guidelines, the diagnosis is made using a combination of major and minor criteria:
Major Criteria:
- Abrupt onset of painful erythematous plaques or nodules
- Histopathology showing dense neutrophilic infiltrate without vasculitis
Minor Criteria (at least two required):
- Fever >38°C
- Association with malignancy, inflammatory disease, or drug exposure
- Leukocytosis
- Excellent response to systemic corticosteroids
- Elevated erythrocyte sedimentation rate (ESR)
(Sources: Cohen PR. Sweet’s syndrome – a comprehensive review of an acute febrile neutrophilic dermatosis. Am J Clin Dermatol. 2007)
Etiology and Triggers
The exact cause of Sweet Syndrome is not fully understood, but several triggers have been identified, including:
- Upper respiratory tract infections
- Autoimmune conditions (e.g., lupus, rheumatoid arthritis)
- Hematologic malignancies (e.g., leukemia)
- Solid tumors
- Medications
Drug-Induced Sweet Syndrome
Several classes of drugs have been linked to Sweet Syndrome, including:
- Antibiotics
- Oral contraceptives
- Colony-stimulating factors
- Antiepileptics
- Antihypertensives
Though rarely associated, this case introduces a potential link between inhaled long-acting bronchodilators and Sweet Syndrome, emphasizing the need for ongoing pharmacovigilance and clinician awareness.
Treatment and Prognosis
The first-line treatment for Sweet Syndrome is systemic corticosteroids (e.g., prednisone), which often result in a rapid resolution of symptoms within a few days.
In refractory or recurrent cases, alternative therapies may include:
- Colchicine
- Dapsone
- Potassium iodide
- Immunosuppressive agents (e.g., cyclosporine, azathioprine)
Early diagnosis and treatment significantly improve outcomes and help prevent systemic involvement.
Differential Diagnosis
Due to its varied presentation, Sweet Syndrome must be distinguished from: